Excessive activation of T cells underlies a range of autoimmune disorders and cancers. Programmed cell death-1 (PD-1) is a protein found on the surface of T cells and can inhibit their activation. When bound to PD-L1 or PD-L2, PD-1 prevents T cell activation and stops excessive immune responses from damaging healthy tissue.
Cancer cells exploit PD-1 to avoid recognition and destruction by the immune system, so PD-1 is an important target for cancer therapeutics. Anti-PD-1 antibodies, such as pembrolizumab and nivolumab, are used successfully as treatments for several types of cancer.
Mechanistically, PD-1 works in opposition to the related protein CD28, another receptor expressed on T cells that promotes T cell activation and survival. While structurally related, PD-1 and CD28 bind different ligands. CD28 pairs up with itself to form a stable homodimer, whereas PD-1 has been thought to operate alone on the surface as a monomer. This difference might be expected to give CD28 the upper hand by 2 to 1.
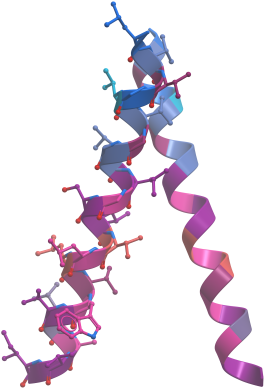
However, a new study published in Science Immunology, has for the first time shown that PD-1 and its ligands also form homodimers. Unlike CD28, where dimerisation is mediated by interactions in the extracellular domain with formation of a covalent bond, the dimerisation of PD-1 is a consequence of transient A-shaped transmembrane domain interaction, which increases its activity and puts it on a level playing field with CD28 through PD-1's own team-work.


 ©
Shutterstock
©
Shutterstock